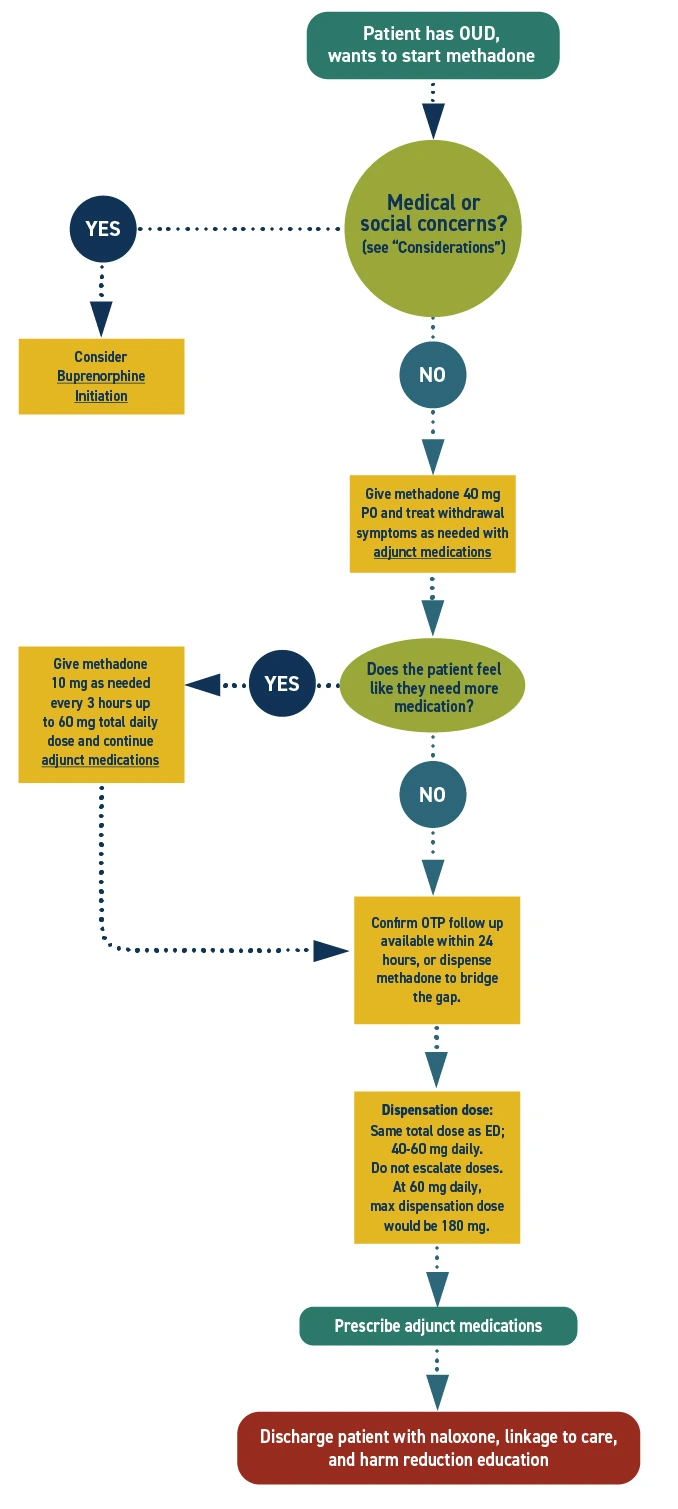
Methadone dispensation
Patient may be dispensed up to a 3-day supply of methadone to bridge the gap between discharge and OTP follow up in accordance with 21 CFR 1306.07(b). Referral to care is required.
Considerations
- Age over 65
- Concurrent sedative use
- COPD with oxygen requirement
- Underlying heart disease (potential for QT prolongation)
Check if the patient can reliably connect with an OTP. Consider how far it is, their transportation options, daily dosing requirements, and whether the OTP is accepting new patients. Make sure the patient understands how the OTP works and what to expect.
Don't start methadone unless the OTP can see the patient within 24 hours or there are available appointments or walk-in slots within 72 hours and your hospital has an established process for methadone dispensation.
Communicate with the OTP. At the very least, provide them with records of when and what dose of methadone was given to the patient.
Consider screening for HIV, HCV, STIs, and mental health comorbidities.
Additional Clinical Guidance
- Opioid use disorder (OUD) is a treatable health condition. It is best treated with methadone or buprenorphine.
- Buprenorphine and methadone are life-saving medications for OUD that reduce the risk of all-cause mortality and overdose death by over 50%.
- Recovery often requires multiple treatment attempts. A repeat encounter is not a treatment failure, but an opportunity to reinitiate potentially life-saving medication.
- If patients continue to use other opioids while on methadone or buprenorphine, a higher dose may be needed to manage their symptoms. Therapeutic dosing should be guided by adequate management of withdrawal and cravings.
- Opioid withdrawal is excruciating. Without swift and adequate intervention, patients may self-direct discharge and be at risk for overdose.
- Patients with OUD are highly stigmatized. Stigma prevents people from seeking care and worsens health outcomes. Providers should challenge biases to provide compassionate, evidence-based care.
Assessment
- Patients must be connected to an OTP to continue care and must be able to return to the OTP daily for dosing. Assess the patient's ability to successfully connect with an opioid treatment program (OTP). Consider factors such as daily dosing requirements and access to care in rural areas. Fully inform the patient of OTP process and expectations.
Labs
- Drug testing is not necessary to initiate treatment for OUD.
- If drug testing is performed for clinical reasons, obtain informed consent.
Pharmacotherapy
- Methadone is a long-acting opioid agonist that lessens withdrawal and cravings to use short-acting opioids.
- Because methadone is a long-acting opioid with cumulative effects, dosing should begin low and be gradually up-titrated over days or weeks until an adequate dose is achieved. Patients commonly experience withdrawal and craving during this time and often benefit from adjunct medications.
- Patients may continue to use other opioids prior to reaching a therapeutic dose of methadone. Neither providers nor patients should judge the efficacy of methadone treatment until after the up-titration period.
Special populations
- If a patient is pregnant, refer to the methadone initiation in pregnancy protocol.
- Patients under age 18 must have written parental consent to start methadone for OUD and should initiate at an opioid treatment program.
Polysubstance use
- Polysubstance use is never a contraindication for initiating methadone or buprenorphine.
Patient safety
- Because methadone is a long-acting opioid with cumulative effects, dosing should begin low and be gradually up-titrated over days or weeks until an adequate dose is achieved. Patients commonly experience withdrawal and craving during this time and often benefit from adjunct medications.
- Patients may continue to use other opioids prior to reaching a therapeutic dose of methadone. Neither providers nor patients should judge the efficacy of methadone treatment until after the up-titration period.
- Methadone can cause respiratory depression when taken at high doses or combined with other sedatives. Patients should not initiate or increase the use of other sedatives, nor should they drink more than their usual amount of alcohol while starting methadone.
- Patients should not drive or operate heavy machinery until they have adjusted to methadone.
Discharge Planning
- Help the patient schedule a follow-up appointment with an OTP. Hospitals enrolled in ScalaNW can call the 24/7 appointment scheduling line and receive a confirmed date, time, and location for MOUD follow up appointment during the 10-minute phone call.
- For hospitals not enrolled in ScalaNW, reference the Washington State Opioid Treatment Program Guide for OTP locations and contact information.
- Ask the patient if they have previously been established with an OTP and where they would like to receive ongoing care.
- Educate the patient on the expectation for daily dosing at an OTP. After some time, they will start to receive take-home doses. Ensure they understand methadone can only be obtained from an OTP and that they have a plan for how to attend appointments.
- Provide the OTP with documentation of the patient's methadone dose, including the date, time, and dosing regimen, if possible. Also give the patient a copy of this information to bring to their OTP appointment.
- 21 CFR 1306.07(b) hospitals to provide methadone to treat opioid withdrawal and initiate medications to treat OUD. Patients can be discharged with up to a 3-day supply of methadone if they are referred to an OTP for ongoing care.
- Many patients need adjunct medications to control withdrawal symptoms until they stabilize on methadone. If needed, provide prescriptions for adjunct withdrawal management medications to cover at least 7 days.
- In Washington, emergency departments are required to dispense naloxone to patients with OUD or others who are at risk of opioid overdose, in compliance with SB5195. Ensure the patient is discharged with naloxone in hand.
- When possible, connect patients with supports such as social workers, care navigators, or peers to improve patient experience and strengthen linkage to care.
Patient Education
Educate the patient about:
- The need to slowly increase methadone dose. Advise patients not to judge its effectiveness until the appropriate dose has been reached.
- Adjunct medications may be required to control withdrawal symptoms. Remind patients that they will not be turned away from the OTP. Even if they use other drugs before their appointment, they can still attend and receive their scheduled dose of methadone.
- Methadone can cause respiratory depression when taken at high doses or combined with other sedatives. Instruct patients not to increase the use of other sedatives and not to drink more than their usual amount of alcohol while starting methadone.
- The importance of avoiding driving or operating machinery until they are accustomed to their medication. Provide work notes if needed.
- Overdose prevention strategies. Ensure the patient and their support system understand when and how to use naloxone.
Discharge Instructions
Information about methadone
- Methadone is a safe and effective medication used to treat opioid use disorder (OUD). Methadone helps people with OUD break the cycle of use and withdrawal, feel more stable, and focus on other parts of their lives so they can recover.
- Methadone significantly lowers the risk of opioid overdose if you take other opioids.
- Stopping methadone will cause withdrawal and increase the risk of opioid overdose if you use other opioids.
- There is no limit to how long a person can take methadone. It is recommended that most people be on the medication long-term.
- Side effects may occur and are typically mild and improve over time. These can include constipation, sweating, headache, dizziness, trouble sleeping, nausea, and sleepiness. If these occur, notify your health care provider, nurse, or pharmacist.
- Over time, your body will adjust to methadone. If you stop taking it suddenly, you will feel withdrawal symptoms within a few days.
- A common side effect of methadone and other opioid medications is constipation. To prevent constipation: stay hydrated, eat plenty of fiber, and start taking an over-the-counter stool softener. If you do not have a bowel movement in over 24-48 hours, try an over-the-counter laxative. Talk to the pharmacist to help choose the best one for you.
Getting methadone
- You can only get methadone from a specialty clinic called an opioid treatment program (OTP).
- At first, you may need to go in person to the OTP every day to receive your dose. Over time, you may be able to take some doses home (take home doses), but you will still need to attend the clinic regularly.
- If you cannot continue care at an OTP, ask your provider about buprenorphine as another option.
CAUTION
- Continue taking your regular methadone dose even if you feel better. Stopping may cause withdrawal and cravings. Your risk of overdose will be much higher if you use opioids without being on this medication.
- Do not start taking or increase your use of other sedative medications like benzodiazepines. The combination of methadone and other sedatives could make you so sleepy that you may stop breathing.
- Do not drink more than your usual amount of alcohol while starting methadone.
- Do not drive when you first start methadone because it may slow your reaction time. Wait until you know how it affects you.
- Remember that changes in opioid use patterns can alter your tolerance and increase your risk of opioid overdose. If you use other opioids, take steps to lower the risk—carry naloxone, never use alone, or call the Never Use Alone lifeline (877-696-1996).
Methadone dose and time taken
________mg @___:____
Overdose Prevention
- Using drugs is risky. If you use, lower your risk of dying from an opioid overdose with the following strategies:
- Naloxone
- Today you received naloxone or a prescription for naloxone. This medication reverses opioid overdose. It is safe to use on anyone you suspect is experiencing an opioid overdose.
- Visit stopoverdose.org or talk to your provider, nurse, or pharmacist to learn more.
- Try not to use alone
- If you are not with other people, connect with a confidential service like neverusealone.com. This peer-led service will send someone to help if you stop responding during a chat or phone call.
- Start low & go slow
- You can't know the full contents or strength of street drugs. If you use, start with a very small amount to see how it affects you.
- Be extra cautious if you have low tolerance (for example, after not using for awhile). If you decide to use more, slowly increase in small amounts.
- Watch and wait before next person uses
- If you’re with a group of people, take turns to see how the drug is affecting people. Someone needs to be able to ask for help.
- Avoid mixing drugs
- Mixing drugs increases your risk. If you use multiple drugs, try to use one at a time and use less of each.
- Know the signs of opioid overdose and how to respond.
- If someone is unresponsive or has unusual or no breathing, call 911 and give them naloxone and rescue breaths.
- Always have naloxone
- Tell others you have it, where it is, and when to use it.
- Treatment with methadone or buprenorphine
- These medications, if taken as directed, lower the risk of death by over 50%.
- If you need help finding a treatment provider, call the Washington Recovery Helpline at 866-789-1511 or go to warecoveryhelpline.org.
Additional Resources
eCFR :: 21 CFR 1306.07 -- Administering or dispensing of narcotic drugs.
References
- American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Opioids, Hatten BW, Cantrill SV, et al. Clinical Policy: Critical Issues Related to Opioids in Adult Patients Presenting to the Emergency Department. Ann Emerg Med. 2020;76(3):e13-e39. doi:10.1016/j.annemergmed.2020.06.049
- American Psychiatric Association. Treatment of opioid use disorder in the general hospital. Approved by the Joint Reference Committee, October 2022. American Psychiatric Association; 2022:59. https://www.psychiatry.org/getattachment/879082d5-af6b-4c26-86e5-152bd53012b5/Resource-Document-Treatment-of-OUD-in-General-Hospital.pdf
- American Society of Addiction Medicine. National practice guideline for the treatment of opioid use disorder 2020 focused update. American Society of Addiction Medicine; 2020.
- Babu KM, Brent J, Juurlink DN. Prevention of Opioid Overdose. N Engl J Med. 2019;380(23):2246-2255. doi:10.1056/NEJMra1807054
- Bowman LA, Berger O, Nesbit S, Stoller KB, Buresh M, Stewart R. Operationalizing the new DEA exception: A novel process for dispensing of methadone for opioid use disorder at discharge from acute care settings. Am J Health Syst Pharm. 2024;81(6):204-218. doi:10.1093/ajhp/zxad288
- Bromley L, Kahan M, Regenstreif L, Srivastava A, Wyman J. Methadone treatment for people who use fentanyl: recommendations. META:PHI; 2021:30. www.metaphi.ca
- Casey S, Regan S, Gale E, et al. Rapid methadone induction in a general hospital setting: a retrospective, observational analysis. Subst Abuse. 2023;44(3):177-183. doi:10.1177/08897077231185655
- Chou R, Cruciani RA, Fiellin DA, et al. Methadone safety: a clinical practice guideline from the American Pain Society and College on Problems of Drug Dependence, in collaboration with the Heart Rhythm Society. J Pain. 2014;15(4):321-337. doi:10.1016/j.jpain.2014.01.494
- Cohen SM, Straus E, Fiellin DA, et al. Hospital-Based Methadone and Buprenorphine Initiation Practices by Addiction Consult Services. JAMA Netw Open. 2025;8(8):e2526077. Published 2025 Aug 1. doi:10.1001/jamanetworkopen.2025.26077
- Crotty K, Freedman KI, Kampman KM. Executive Summary of the Focused Update of the ASAM National Practice Guideline for the Treatment of Opioid Use Disorder. J Addict Med. 2020;14(2):99-112. doi:10.1097/ADM.0000000000000635
- Englander H, Thakrar AP, Bagley SM, Rolley T, Dong K, Hyshka E. Caring for Hospitalized Adults With Opioid Use Disorder in the Era of Fentanyl: A Review. JAMA Intern Med. 2024;184(6):691-701. doi:10.1001/jamainternmed.2023.7282
- Huo S, Heil J, Salzman MS, Carroll G, Haroz R. Methadone initiation in the emergency department for opioid use disorder: a case series. J Emerg Med. 2023;64(3):391-396. doi:10.1016/j.jemermed.2023.01.012
- Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use. J Addict Med. 2015;9(5):358-367. doi:10.1097/ADM.0000000000000166
- Methadose. Package insert. SPECGX LLC; Accessed August 15, 2025. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=017116
- Racha S, Patel SM, Bou Harfouch LT, Berger O, Buresh ME. Safety of rapid inpatient methadone initiation protocol: a retrospective cohort study. J Subst Use Addict Treat. 2023;148:209004. doi:10.1016/j.josat.2023.209004
- Schoenfeld EM, Westafer LM, Beck SA, et al. "Just give them a choice": patients' perspectives on starting medications for opioid use disorder in the ED. Acad Emerg Med. 2022;29(8):928-943. doi:10.1111/acem.14507
- Schuckit MA. Treatment of Opioid-Use Disorders. N Engl J Med. 2016;375(4):357-368. doi:10.1056/NEJMra1604339
- Volkow ND, Jones EB, Einstein EB, Wargo EM. Prevention and Treatment of Opioid Misuse and Addiction: A Review. JAMA Psychiatry. 2019;76(2):208-216. doi:10.1001/jamapsychiatry.2018.3126


 I’M A CLINICIAN
I’M A CLINICIAN I’M A PATIENT
I’M A PATIENT