Considerations
Higher doses of buprenorphine have been found to be very safe in the adult population and lower the risk of precipitated withdrawal.
The lower the COWS score the higher the risk of precipitated withdrawal. Active stimulant intoxication can falsely elevate the COWS score. The use of buprenorphine can unmask symptoms of stimulant intoxication.
Providers should engage in shared decision making with the patient.
Potential complicating factors include:
- Allergy or sensitivity
- Severe respiratory compromise
- Chronic use of long acting opioids (e.g., methadone or Oxycontin®)
Consider expert consultation, but prioritize treating symptoms.
Consider screening for HIV, HCV, STIs, and mental health comorbidities. Link to ongoing care as needed.
Additional Clinical Guidance
- Opioid use disorder (OUD) is a treatable health condition. It is best treated with methadone or buprenorphine.
- Buprenorphine and methadone are life-saving medications for OUD that reduce the risk of all-cause mortality and overdose death by over 50%.
- Recovery often requires multiple treatment attempts. A repeat encounter is not a treatment failure, but an opportunity to reinitiate potentially life-saving medication.
- If patients continue to use other opioids while on methadone or buprenorphine, a higher dose may be needed to manage their symptoms. Therapeutic dosing should be guided by adequate management of withdrawal and cravings.
- Opioid withdrawal is excruciating. Without swift and adequate intervention, patients may self-direct discharge and be at risk for overdose.
- Patients with OUD are highly stigmatized. Stigma prevents people from seeking care and worsens health outcomes. Providers should challenge biases to provide compassionate, evidence-based care.
Assessment
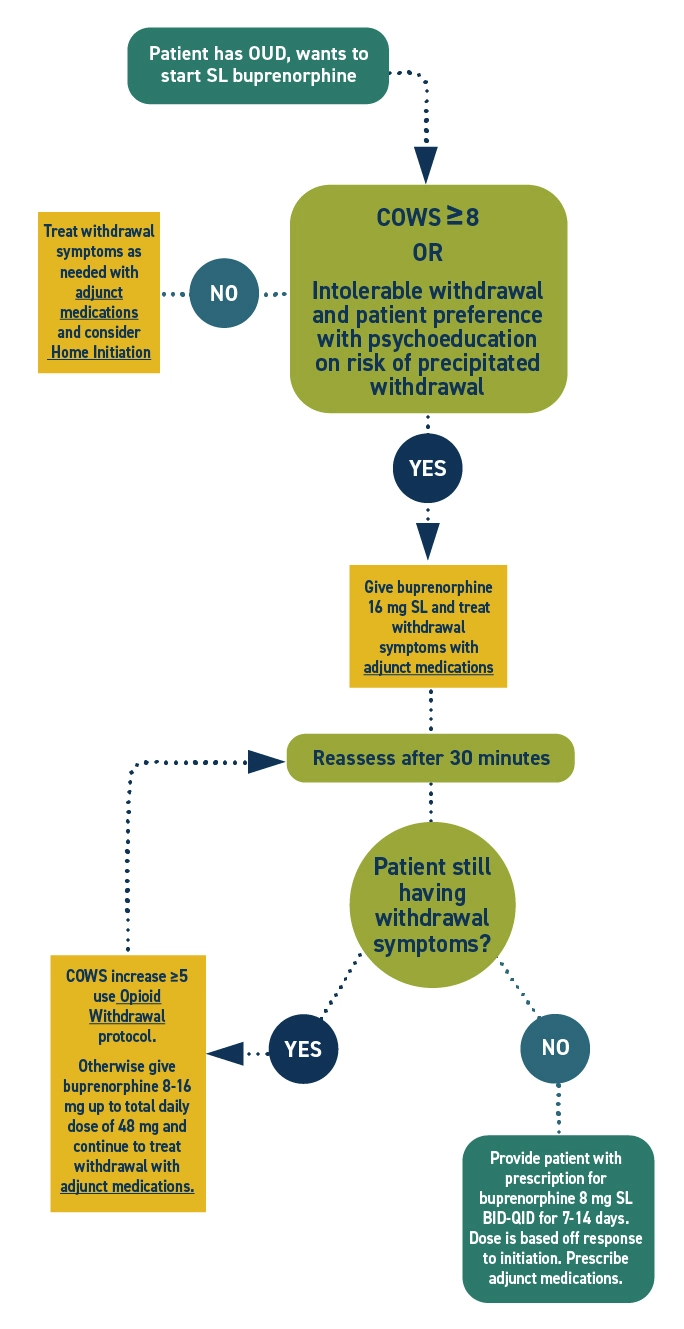
- Assess the Clinical Opiate Withdrawal Scale (COWS) score before administering buprenorphine. For this initiation approach, only administer buprenorphine if the patient has signs of withdrawal.
- Reassess vitals, COWS, and subjective experience of withdrawal within 30 minutes of buprenorphine administration.
Labs
- Drug testing is not necessary to initiate treatment for OUD.
- If drug testing is performed for clinical reasons, obtain informed consent.
Pharmacotherapy
- Buprenorphine is a partial opioid agonist that helps to minimize withdrawal and lessen opioid cravings.
- Buprenorphine has minimal effect on respiratory drive, making respiratory depression unlikely even at higher doses.
- Buprenorphine has high receptor affinity, allowing it to out-compete other opioids. This competitive binding can precipitate withdrawal because it will rapidly replace the more potent opioid that is present. This is why patients should be in withdrawal before starting buprenorphine with this method.
- Competitive binding also reduces overdose risk by blocking other opioids. Even a single dose provides protection for at least 24 hours, during the high-risk period after discharge.
- Doses should be adjusted based on symptoms— if the patient has ongoing withdrawal symptoms or cravings to use, a dose increase should be considered.
Special populations
- If a patient is pregnant, refer to the care of OUD in pregnancy protocol.
- If a patient is under 18, refer to the buprenorphine initiation in adolescents protocol.
Polysubstance use
- Active stimulant intoxication can falsely elevate the COWS score.
- Buprenorphine administration may unmask symptoms of stimulant intoxication.
- Polysubstance use is never a contraindication for initiating buprenorphine or methadone.
Administration
- Because buprenorphine is a partial agonist, if the first dose is administered too soon after recent full agonist opioid use in a patient with opioid dependence, there is a risk of precipitated withdrawal. This is a sudden worsening of withdrawal symptoms after buprenorphine administration. If this occurs, give additional doses of buprenorphine and adjunct medications to alleviate withdrawal symptoms.
- Inform the patient of the risk of precipitated withdrawal. Ask them to report right away if their symptoms worsen, reassure them that they will receive immediate treatment if this occurs.
- Administering buprenorphine:
- Buprenorphine comes in film and tablet forms, and both must be taken sublingually. The medication is poorly absorbed in the stomach. It must be taken correctly to receive the benefit.
- The patient should let the medication dissolve fully under their tongue. This typically takes 5-10 minutes, but sometimes longer. Drinking water prior to administration can help it dissolve faster. Many patients find the taste unpleasant. One way to know that the medication is dissolved and absorbed is when the taste subsides.
- Patients should not eat, drink, or talk while the medication is dissolving.
- To prevent oral decay, instruct the patient to rinse their mouth with water 30 minutes after administration.
Discharge planning
- Help the patient schedule a follow-up appointment. Hospitals enrolled in ScalaNW can call the 24/7 appointment scheduling line and receive a confirmed date, time, and location for MOUD follow up appointment during the 10-minute phone call.
- For hospitals not enrolled in ScalaNW, the Washington Recovery Helpline MOUD Locator (online or at 1-866-789-1511) is a useful resource for finding OUD treatment in Washington.
- Provide the patient with a buprenorphine prescription to last until their scheduled outpatient appointment. When possible, prescribe 3 additional days beyond the appointment date to allow for barriers or rescheduling. If no appointment is scheduled, provide at least 7-14 days of medication to give the patient time to secure an appointment.
- Patients can call the Washington Telebuprenorphine Hotline (206-289-0287) if they run out of medication prior to their follow up appointment.
- Provide the patient with discharge instructions that include the time of the last dose and when to take the next dose. Ensure the patient understands the importance of taking buprenorphine at around the same time every day.
- Many patients need adjunct medications to control withdrawal symptoms until they stabilize on buprenorphine. If needed, provide prescriptions for adjunct withdrawal.
- In Washington, emergency departments are required to dispense naloxone to patients with OUD or others who are at risk of opioid overdose, in compliance with SB5195. Ensure patient is discharged with naloxone in hand.
- When possible, connect patients with supports such as social workers, care navigators, or peers to improve patient experience and strengthen linkage to care.
Patient Education
Educate the patient about:
- Buprenorphine administration
- Must be administered under the tongue for proper absorption.
- It can take 5-10 minutes for the medication to fully absorb. Avoid eating, drinking, smoking, or talking during this time.
- Drinking water prior to administration can help it dissolve faster.
- To prevent oral decay, rinse mouth with water 30 minutes after administration.
- The risks of combining sedatives with buprenorphine, which can cause respiratory depression.
- The importance of avoiding driving or operating machinery until accustomed to the medication. Provide work notes if needed.
- Overdose prevention strategies. Ensure the patient and their support system understand when and how to use naloxone.
- The risks of change in use patterns, which can alter tolerance and increase risk of opioid overdose.
Discharge Instructions
Information about buprenorphine
- Buprenorphine is a safe and effective medication used to treat opioid use disorder (OUD).
- Buprenorphine helps people with OUD break the cycle of use and withdrawal, feel more stable, and focus on other parts of their lives so they can recover.
- When used as prescribed, buprenorphine significantly lowers the risk of opioid overdose if you take other opioids.
- There are two kinds of buprenorphine. Buprenorphine-naloxone also contains naloxone. Naloxone is not absorbed when the medication is taken as directed (under the tongue). If the medication is injected, however, the naloxone will be absorbed and can cause severe opioid withdrawal.
- There is no limit to how long a person can take buprenorphine. It is recommended that most people be on the medication long-term.
- Side effects may occur and are typically mild and improve over time. These can include constipation, sweating, headache, dizziness, trouble sleeping, nausea, and sleepiness. If these occur, notify your health care provider, nurse, or pharmacist.
- Over time, your body will adjust to buprenorphine. If you stop taking it suddenly, you will feel withdrawal symptoms within a few days.
- A common side effect of buprenorphine and other opioid medications is constipation. To prevent constipation: stay hydrated, eat plenty of fiber, and start taking an over-the-counter stool softener. If you do not have a bowel movement in over 24-48 hours, try an over-the-counter laxative. Talk to the pharmacist to help choose the best one for you.
How to take buprenorphine
- You will receive buprenorphine in either film or tablet form.
- Do not swallow the medicine. It will not work if swallowed.
- Place the medication under your tongue and allow it to fully dissolve. This can take 5-15 minutes.
- Drinking water before taking buprenorphine may help it dissolve faster.
- Do not drink water while the medication is under your tongue.
- Do not eat, drink, talk, or smoke while the medication is dissolving.
- After the medication has dissolved, do not smoke, eat, or drink for at least 15 minutes.
- To prevent tooth decay, rinse your mouth with water 30 minutes after taking the medication.
CAUTION
- Continue taking your regular buprenorphine dose, even if you feel better. Stopping may cause withdrawal and cravings. Your risk of overdose will be much higher if you use opioids without being on this medication.
- Do not start taking or increase your use of other sedative medications like benzodiazepines. The combination of buprenorphine and other sedatives could make you so sleepy that you may stop breathing.
- Do not drink more than your usual amount of alcohol while starting buprenorphine.
- Do not drive when you first start buprenorphine because it may slow your reaction time. Wait until you know how it affects you.
- Remember that changes in opioid use patterns can alter your tolerance and increase your risk of opioid overdose. If you use other opioids, take steps to lower the risk—carry naloxone, never use alone, or call the Never Use Alone lifeline (877-696-1996).
Buprenorphine dose and time taken
________mg @___:____
Overdose Prevention
- Using drugs is risky. If you use drugs, lower your risk of dying from an opioid overdose with the following strategies:
- Naloxone
- Today you received naloxone or a prescription for naloxone. This is an opioid overdose reversal medication. It is safe to use on anyone you suspect is experiencing an opioid overdose.
- Visit stopoverdose.org or talk to your provider, nurse, or pharmacist to learn more.
- Try not to use alone
- If you are not with other people, connect with a confidential service like neverusealone.com. This peer-led service will send someone to help if you stop responding during a chat or phone call.
- Start low & go slow
- You can't know the full contents or strength of drugs. If you use, start with a very small amount to see how it affects you.
- Be extra cautious if you have low tolerance (for example, after not using for awhile). If you decide to use more, slowly increase in small amounts.
- Watch and wait before next person uses
- If you’re with a group of people, take turns to see how the drug is affecting people. Someone needs to be able to ask for help.
- Avoid mixing drugs
- Mixing drugs increases your risk. If you use multiple drugs, try to use one at a time and use less of each.
- Know the signs of opioid overdose and how to respond.
- If someone is unresponsive or has unusual or no breathing, call 911 and give them naloxone and rescue breaths.
- Always have naloxone
- Tell others you have it, where it is, and when to use it.
- Treatment with methadone or buprenorphine
- These medications, if taken as directed, lower the risk of death by over 50%.
- If you need help finding a treatment provider, call the Washington Recovery Helpline at 866-789-1511 or go to warecoveryhelpline.org.
References
- American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Opioids, Hatten BW, Cantrill SV, et al. Clinical policy: critical issues related to opioids in adult patients presenting to the emergency department. Ann Emerg Med. 2020;76(3):e13-e39. doi:10.1016/j.annemergmed.2020.06.049
- American Psychiatric Association. Treatment of opioid use disorder in the general hospital. Approved by the Joint Reference Committee, October 2022. American Psychiatric Association; 2022:59. https://www.psychiatry.org/getattachment/879082d5-af6b-4c26-86e5-152bd53012b5/Resource-Document-Treatment-of-OUD-in-General-Hospital.pdf
- American Society of Addiction Medicine. National practice guideline for the treatment of opioid use disorder 2020 focused update. American Society of Addiction Medicine; 2020.
- Axeen S, Pacula RL, Merlin JS, Gordon AJ, Stein BD. Association of daily doses of buprenorphine with urgent health care utilization. JAMA Netw Open. 2024;7(9):e2435478.
- Babu KM, Brent J, Juurlink DN. Prevention of opioid overdose. N Engl J Med. 2019;380(23):2246-2255. doi:10.1056/NEJMra1807054
- Chambers LC, Hallowell BD, Zullo AR, et al. Buprenorphine dose and time to discontinuation among patients with opioid use disorder in the era of fentanyl. JAMA Netw Open. 2023;6(9):e2334540.
- Crotty K, Freedman KI, Kampman KM. Executive summary of the focused update of the ASAM National Practice Guideline for the treatment of opioid use disorder. J Addict Med. 2020;14(2):99-112. doi:10.1097/ADM.0000000000000635
- D'Onofrio G, O'Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636-1644. doi:10.1001/jama.2015.3474
- Dekker AM, Schriger DL, Herring AA, Samuels EA. Emergency clinician buprenorphine initiation, subsequent prescriptions, and continuous prescriptions. JAMA. Published online February 19, 2025. doi:10.1001/jama.2024.27976
- Englander H, Thakrar AP, Bagley SM, Rolley T, Dong K, Hyshka E. Caring for hospitalized adults with opioid use disorder in the era of fentanyl: a review. JAMA Intern Med. 2024;184(6):691-701. doi:10.1001/jamainternmed.2023.7282
- Grande LA, Cundiff D, Greenwald MK, Murray M, Wright TE, Martin SA. Evidence on buprenorphine dose limits: a review. J Addict Med. 2023;17(5):509-516.
- Herring AA, Perrone J, Nelson LS. Managing opioid withdrawal in the emergency department with buprenorphine. Ann Emerg Med. 2019;73(5):481-487.
- Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use. J Addict Med. 2015;9(5):358-367. doi:10.1097/ADM.0000000000000166
- Providers Clinical Support System. Practice-based guidelines: buprenorphine in the age of fentanyl. Published 2023. Accessed August 15, 2025.
https://pcssnow.org/wp-content/uploads/2023/05/PCSS-Fentanyl-Guidance-FINAL-1.pdf - Schoenfeld EM, Westafer LM, Beck SA, et al. "Just give them a choice": patients' perspectives on starting medications for opioid use disorder in the ED. Acad Emerg Med. 2022;29(8):928-943. doi:10.1111/acem.14507
- Weimer MB, Herring AA, Kawasaki SS, Meyer M, Kleykamp BA, Ramsey KS. ASAM clinical considerations: buprenorphine treatment of opioid use disorder for individuals using high-potency synthetic opioids. J Addict Med. 2023;17(6):632-639.
- Weiner SG, Baker O, Bernson D, Schuur JD. One-year mortality of patients after emergency department treatment for nonfatal opioid overdose. Ann Emerg Med. 2020;75(1):13-17.
- Wong S, Fabiano N, Webber D, Kleinman RA. High-dose buprenorphine initiation: a scoping review. J Addict Med. 2024;18(4):349-359. doi:10.1097/ADM.0000000000001296


 I’M A CLINICIAN
I’M A CLINICIAN I’M A PATIENT
I’M A PATIENT