Considerations
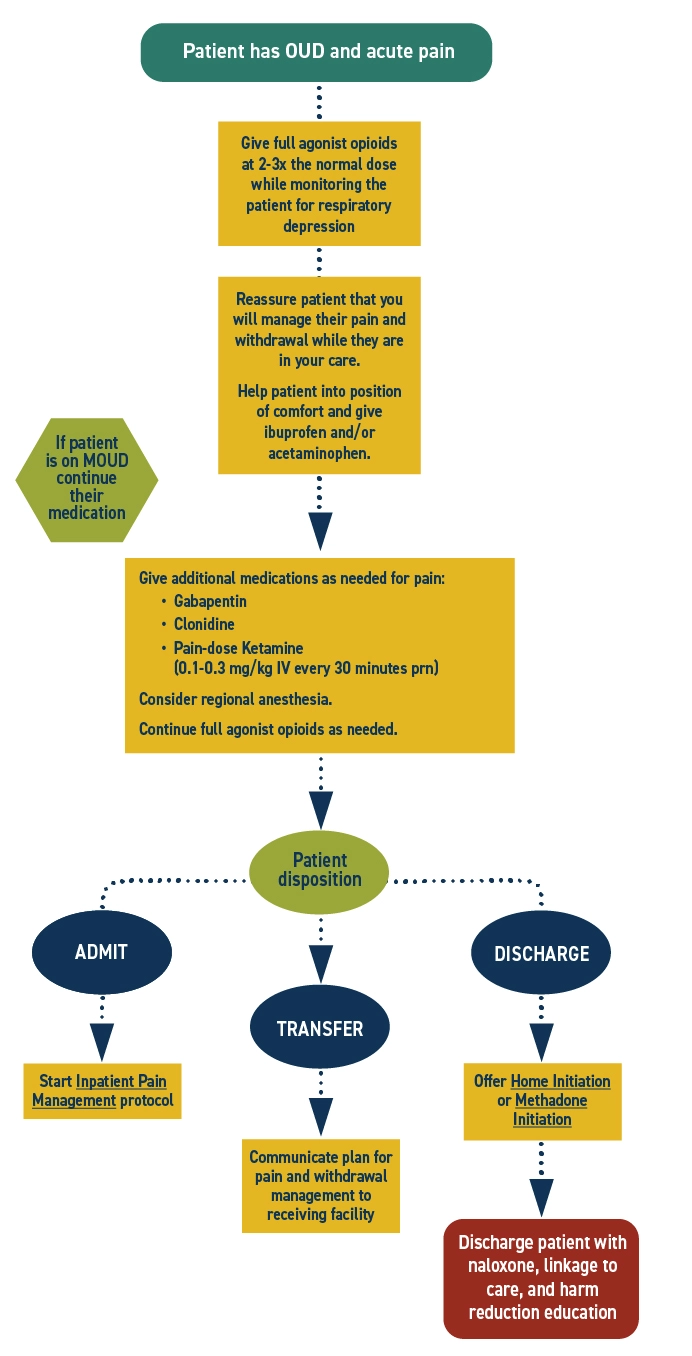
Opioids for analgesia will need to be given at higher doses due to opioid tolerance in patients with OUD, often 2-3x the usual dose to adequately control pain.
The risk of respiratory depression in this case is low. If respiratory rate remains within normal limits and the patient is not overly sedated, the dose is not too high.
Treating an acute painful condition does not worsen a patient's OUD.
Full agonist, short-acting opioids for pain can be used in addition to buprenorphine or methadone for opioid use disorder (OUD).
This protocol does not cover the care of patients on naltrexone. Consider expert consultation.
Additional Clinical Guidance
- Acute pain is treatable and should be managed in patients with opioid use disorder (OUD). Untreated or undertreated pain may prevent patients from completing needed medical care, cause physical and psychological harm, and place patients at high risk for overdose.
- Evidence supports treating both OUD and pain simultaneously. Methadone and buprenorphine should be maintained or can be initiated during an acute pain episode such as post-op, injury, or trauma. Full agonist opioids can be safely used and titrated to relieve pain.
- MOUD initiation should never be a requirement for adequate pain management. Full agonist opioid use does not worsen or enable opioid use disorder.
- Patients with OUD are highly stigmatized. Stigma prevents people from seeking care or reaching out for help when they need it. Providers should reflect on and challenge biases to provide compassionate and evidence-based care that improves outcomes.
Assessment
- Ask the patient about the type, amount, and frequency of opioids they are currently taking. This can help gauge how much opioid pain management they need. However, this information is relative and the contents and doses of drugs are highly variable.
- Many patients will experience anxiety related to undertreated pain. It is vital to treat patients in a caring and supportive manner and regularly reassess their pain. Communicate with the patient and use shared decision making to create a plan if their pain is not well controlled.
Pharmacotherapy
- Patients taking opioid agonist medications for OUD should continue their regular dose throughout their stay to improve outcomes.
- Treating pain often requires a multimodal approach. Additional pharmacological and non-pharmacological pain management should be explored. Adjunctive medications such as NSAIDs, acetaminophen, hydroxyzine, or clonidine may also reduce the dose of opioid needed to control pain.
- Methadone
- As a full agonist, methadone provides baseline OUD symptom control and does not block receptors.
- Short-acting opioids will bind freely and should be titrated to overcome tolerance for adequate pain control.
- Buprenorphine
- As a partial agonist, buprenorphine partially blocks receptors. It also has high receptor affinity.
- Even at high buprenorphine doses, full agonists can displace it when given at high enough doses.
- Opioids for analgesia will need to be given at higher doses than normal to outcompete buprenorphine to occupy opioid receptors.
- Increasing the daily dose of buprenorphine and/or split dosing may better control pain than a once daily dose.
- Naltrexone
- This protocol does not cover the care of patients on naltrexone. Consider expert consultation.
Patient safety
- Patients taking opioid agonist medications for OUD should continue their regular dose throughout their stay to improve outcomes.
Discharge planning
- If the patient is discharged with an additional prescription opioid, ensure they continue to take their methadone or buprenorphine and have a plan to discontinue the short-term opioid. Patients may need additional support with medication management during this time.
- If the patient is on sublingual buprenorphine and is not prescribed an additional opioid at discharge, consider the option of split dosing to manage pain. Educate the patient on additional pain management options such as over-the-counter medications and non-pharmacological interventions.
- In Washington, emergency departments are required to dispense naloxone to patients with OUD or others who are at risk of opioid overdose in compliance with SB5195. Ensure patient is discharged with naloxone in hand.
- When possible, connect patients with supports such as social workers, care navigators, or peers to improve patient experience and strengthen linkage to care.
Discharge Instructions
- Continue taking buprenorphine or methadone at your regular dose. It is okay to take this medication along with the other medications you were prescribed today.
- Tell your buprenorphine or methadone provider that you have a painful condition and what medications you were given today. It is common for people on medications for opioid use disorder to need additional medications when they have severe pain.
- Use other pain management strategies as well, including getting into a comfortable position, using heat, cold, and over-the-counter medications like acetaminophen and ibuprofen.
- Remember that changes in use patterns can alter tolerance and increase your risk of opioid overdose. If you use other opioids, take steps to reduce the risk associated with overdose, like having naloxone, not using alone or calling the Never Use Alone lifeline (877-696-1996), and starting low and going slow.
References
- American Psychiatric Association. Treatment of opioid use disorder in the general hospital. Approved by the Joint Reference Committee, October 2022. American Psychiatric Association; 2022:59. https://www.psychiatry.org/getattachment/879082d5-af6b-4c26-86e5-152bd53012b5/Resource-Document-Treatment-of-OUD-in-General-Hospital.pdf
- Crotty K, Freedman KI, Kampman KM. Executive summary of the focused update of the ASAM National Practice Guideline for the treatment of opioid use disorder. J Addict Med. 2020;14(2):99-112. doi:10.1097/ADM.0000000000000635
- De Aquino JP, Parida S, Avila-Quintero VJ, et al. Opioid-induced analgesia among persons with opioid use disorder receiving methadone or buprenorphine: A systematic review of experimental pain studies. Drug Alcohol Depend. 2021;228:109097. doi:10.1016/j.drugalcdep.2021.109097
- Englander H, Thakrar AP, Bagley SM, Rolley T, Dong K, Hyshka E. Caring for hospitalized adults with opioid use disorder in the era of fentanyl: a review. JAMA Intern Med. 2024;184(6):691-701. doi:10.1001/jamainternmed.2023.7282
- Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use. J Addict Med. 2015;9(5):358-367. doi:10.1097/ADM.0000000000000166
- Merlin JS, Khodyakov D, Arnold R, et al. Expert Panel Consensus on Management of Advanced Cancer-Related Pain in Individuals With Opioid Use Disorder. JAMA Netw Open. 2021;4(12):e2139968. Published 2021 Dec 1. doi:10.1001/jamanetworkopen.2021.39968
- Thakrar AP, Lowenstein M, Greysen SR, Delgado MK. Trends in Before Medically Advised Discharges for Patients With Opioid Use Disorder, 2016-2020. JAMA. 2023;330(23):2302-2304. doi:10.1001/jama.2023.21288
- Veazie S, Mackey K, Peterson K, Bourne D. Managing Acute Pain in Patients Taking Medication for Opioid Use Disorder: a Rapid Review. J Gen Intern Med. 2020;35(Suppl 3):945-953. doi:10.1007/s11606-020-06256-5


 I’M A CLINICIAN
I’M A CLINICIAN I’M A PATIENT
I’M A PATIENT